Community based research project: CHILDHOOD OBESITY
Childhood obesity is when a child is above the ‘normal’ weight for their height and age, meaning he/she carries abnormal amounts of body fat. This is caused when consumption of victuals1 outweighs physical activity (PA) levels2. This is a serious public health issue of the 21st century, with one in four Australian children either overweight or obese ("Childhood obesity", 2018). An individual classified as overweight or obese has substantially higher risk of life-threatening diseases such as cardiovascular disease, type II diabetes and many others. There is around an 80% chance of an obese child developing obesity during adulthood, which increases the individuals risks of illness and premature death ("Childhood overweight and obesity: evidence, prevention and response", 2019).
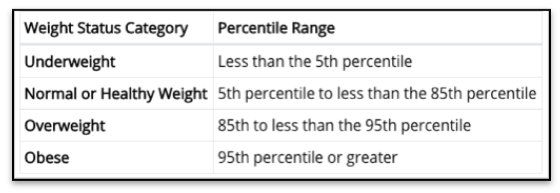
Figure one: BMI weight categories for children and teens (Defining Childhood Obesity | Overweight & Obesity | CDC. (n.d.). Retrieved from https://www.cdc.gov/obesity/childhood/defining.html)
MEASURING CHILDHOOD OBESITY HEALTH ISSUES
Obesity can be diagnosed through tests such as BMI3, waist circumference and other measures performed by medical professionals. BMI is the most popular tool for diagnosis of obesity, measuring an individual’s body mass compared to body height, displayed as Kg/m2 and measured at percentiles (figure one)4. Reaching an overweight or obese percentile for children can be caused by many factors, such as; ‘unhealthy food choices, lack of PA and family eating habits’5(Department of Health & Human Services, 2013). It has been shown that the ‘energy gap’6 for children is much smaller than adults. Meaning a child is able to consume a slighter number of excess calories to maintain a healthy weight, than an adult.7 Because this gap is so small, it is imperative that parents are cautious to ensure their child is consuming the recommended amounts of energy and living a physically active lifestyle.
Obesity during childhood has been shown to have strong association with health issues later in life. Some of these issues include; obesity, type II diabetes and heart disease8. ("Childhood overweight and obesity", 2017)
While an obese person is not guaranteed to develop one/all of these concerns, it has been recognized they are at higher risk than a person of healthy weight.
INFLUENCING FACTORS
There are many factors which may influence childhood obesity, such as:
Diet and lifestyle
The ultimate cause of childhood obesity is excessive consumption of energy dense foods, paired with low levels of PA ("Childhood overweight and obesity", 2017). A healthy child should be consuming a wide range of nutritious foods such as; fruits, vegetables, meats and dairy products, with limited saturated fat intake, foods low in salt and low amounts of sugars and added sugars ("Healthy eating for children", November, 2017). A child9 should also be completing at least 60 minutes of moderate-vigorous PA everyday and limit sedentary behaviour as much as possible (Australian PA and sedentary behaviour guidelines). Following these guidelines will help prevent obesity in children.
Social determinants
Income, socioeconomic status, and education are all factors which may lead to or prevent childhood obesity. Globally, the areas with the highest rates of childhood obesity are low-middle income countries, especially within urban areas ("Childhood overweight and obesity", 2017). This may be due to many reasons such as; lack of education towards nutritional needs, poor access to healthy foods13 or poor employment which leads to lower income, may making it hard to afford fresh, nutritious foods.
Culture, religion and social
The way a person is brought up, including their culture, religion and society can influence their beliefs and traditions toward foods, PA and lifestyle. What a cultural group deems to be an acceptable way of eating and how they appear is totally unique to other cultures. For example, ‘There are some cultures that see being overweight as a sign of affluence because food may be scarce in that region’ (Rubin, 2016). This therefore means different cultures would have varied views or likelihoods of developing obesity.
Access and Food deserts
If a child does not have access to healthy, fresh, nutritious food, they are less likely to consume it, therefore are more likely to develop obesity. This is often the parent/guardian’s responsibility, to provide the child with adequate food choices. If there physically is little/no affordable or good-quality fresh food available to buy in an urban area, this is known as a food desert.
Vulnerability
Genetics can play a large roll in childhood obesity. Some genes may act together to make children more susceptible to developing obesity. Genetic diseases such as Prader-Willi syndrome10 or Cushing’s syndrome11 may increase a child’s likelihood of being obese.
Health literacy
A poor education of nutritional health may lead to a higher risk of developing obesity. If a child cannot determine healthy food or drink choices or perform PA to an acceptable level due to lack of education, they are more likely to become obese.
ACTIVE KIDS INITIATIVE

Results from the Active Kids Program, 2018 ((Jennifer.anderson, 2017).
‘Active Kids’ is a NSW health initiative with an aim reducing childhood obesity12 and increasing the health of children in NSW schools by making them more physically active. It works by a parent registering their child to the ‘Active Kids Program’, which then provides them with a $100 voucher to use throughout the year to ‘cover participation and membership costs for sport, fitness and recreational active
ities’ (Jennifer.anderson, 2017). The initiative began in 2018 and will continue until 2021, meaning parents with kids signed up to the program will receive $100 per year. There are over 9,500 providers associated with the Active Kids program, where parents can use their $100 credit for their kids to ‘swim, twirl, jump, kick and hurdle their way into loads of sport and active recreation activities’ (Jennifer.anderson, 2017).
It is likely the Active Kids program will be successful due to so many sporting organisations (9367 in 2018) involved across NSW as well as a high number of parents and kids redeeming and using their vouchers. This can be seen by the results of the program from 2018, (shown in figure 2) with 638,902 vouchers created and 498,554 vouchers redeemed. This proves large numbers of kids across NSW are getting active because of the program.
CONCLUSION:
Childhood obesity is something that must be monitored in our society today, in effort to increase the health of children and adults in the future. With such a strong association between childhood obesity leading to poor health of adolescents and adults, efforts need to be made to prevent the obesity of children to begin with. Initiatives such as the ‘Active Kids’ program are working towards minimising obesity in children and improving their activity levels and health, setting the children up with a more healthy, active lifestyle.
APPENDIX:
1. Victuals - Food or provisions((n.d.). Retrieved from https://www.google.com/search?q=Dictionary#dobs=victual
2. As well as growing processes and other bodily functions
3. Body mass index
4. A normal range for a child or teen is above the 5th and below the 85th percentile. Overweight is considered between 85th-95th and obese is 95th percentile or above ("Defining Childhood Obesity | Overweight & Obesity | CDC", 2018). (as shown in figure one).
5. For example, if a child lives a sedentary lifestyle and excessively consumes food and drink, it is likely they will become overweight or obese.
6. ‘The term “energy gap” was coined to estimate the change in energy intake andenergy expenditure behaviors required to achieve different body weight outcomes in individuals and populations’ (Hill, Peters, & Wyatt, 2009)
7. For a child to gain unhealthy amounts of weight; they only need to consume approximately 200-300 kilojoules (kj) excess above the recommended 8700 kj per day ("Childhood overweight and obesity: evidence, prevention and response", 2019).
8. As well as; cancer, sleep apnoea, joint problems, emotional and social problems, poor body image, infertility, respiratory disorders and liver problems
9. A child aged 5-12 years
10. Prader-Willi syndrome (PWS) is a genetic disorder that occurs in approximately one out of every 15,000 births. PWS is recognized as the most common genetic cause of life-threatening childhood obesity. ((Fpwr, "About Prader-Willi Syndrome | Foundation for Prader-Willi Research")
11. Cushing's syndrome is caused by a pituitary tumour leading to excessive production of ACTH (adrenocorticotropic hormone). Excessive ACTH stimulates the adrenal cortex to produce high levels of cortisol, producing the disease state. ("Cushing's syndrome", 2019) A common symptom of Crushing’s syndrome is abdominal obesity.
12. Reducing childhood obesity of children aged 4.5-18 years
13. As well as easy access to unhealthy food, such as fast food restaurants
REFERENCES:
1. Childhood overweight and obesity. (2017, October 13). Retrieved from https://www.who.int/dietphysicalactivity/childhood/en/
2. Childhood obesity. (2018, December 17). Retrieved from https://raisingchildren.net.au/school-age/nutrition-fitness/common-concerns/child-obesity
3. Department of Health & Human Services. (2013, April 30). Obesity in children - causes. Retrieved from https://www.betterhealth.vic.gov.au/health/healthyliving/obesity-in-children-causes
4. (n.d.). Retrieved from https://healthywa.wa.gov.au/Articles/N_R/Overweight-and-obesity-in-children
5. Obesity diagnosis (including BMI). (n.d.). Retrieved from https://www.healthdirect.gov.au/obesity-diagnosis
6. Defining Childhood Obesity | Overweight & Obesity | CDC. (n.d.). Retrieved from https://www.cdc.gov/obesity/childhood/defining.html
7. Childhood overweight and obesity: Evidence, prevention and response. (n.d.). Retrieved from http://www.phrp.com.au/issues/march-2019-volume-29-issue-1/childhood-overweight-and-obesity-evidence-prevention-and-response/
8. What is Childhood Obesity? Who is at Risk? (n.d.). Retrieved from https://childhoodobesityfoundation.ca/what-is-childhood-obesity/
9. Food for Health: Dietary Guidelines for Children and Adolescents in Australia. (n.d.). Retrieved from http://www.health.gov.au/internet/publications/publishing.nsf/Content/gug-family-toc~gug-family-guidelines
10. Welcome to the Department of Health. (n.d.). Retrieved from http://www.health.gov.au/
11. Rubin A. (2016, February 11). Health Beat. Is Obesity Culturally Influenced ?Retrieved May 17, 2019, from https://jamaicahospital.org/newsletter/?p=3038
12. How Your Culture Affects Your Weight. (n.d.). Retrieved from https://www.psychologytoday.com/au/blog/cravings/201605/how-your-culture-affects-your-weight
13. Fpwr. (n.d.). About Prader-Willi Syndrome | Foundation for Prader-Willi Research. Retrieved from https://www.fpwr.org/about-prader-willi-syndrome
14. Cushing's syndrome. (2019, April 23). Retrieved from https://en.wikipedia.org/wiki/Cushing's_syndrome
15. Jennifer.anderson. (2017, June 16). Active Kids. Retrieved from https://sport.nsw.gov.au/sectordevelopment/activekids
16. (n.d.). Retrieved from https://www.google.com/search?q=Dictionary#dobs=victual
17. Hill, J. O., Peters, J. C., & Wyatt, H. R. (2009, November). Using the energy gap to address obesity: A commentary. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2796109/
